How I Track My Recovery Every Day — Simple Moves That Actually Help
Recovering from an injury or surgery can feel slow and frustrating. I’ve been there — stuck wondering if I was doing enough, or too much. That’s when I started tracking my rehab progress daily, not just going through the motions. It changed everything. With simple monitoring habits, I saw real improvements, stayed motivated, and avoided setbacks. This is how I made rehab work — not perfectly, but consistently. What began as a personal experiment turned into a reliable system that helped me regain strength, restore mobility, and rebuild trust in my body. It wasn’t about pushing harder; it was about paying attention. And that shift in mindset made all the difference in my healing journey.
The Frustration Behind My Rehab Journey
For weeks after my knee surgery, I followed the physical therapist’s instructions faithfully. I did the prescribed stretches, practiced walking with support, and avoided activities that might strain the joint. Yet progress felt invisible. One day blurred into the next, and I couldn’t tell if I was improving or just maintaining. I remember standing in front of the mirror, trying to bend my knee slightly more than the day before, only to feel discouraged when no change seemed apparent. The absence of measurable feedback made me question my effort — was I doing too little? Or worse, was I doing too much and unknowingly causing harm?
This emotional limbo is common in recovery. Many people assume that simply completing exercises means progress, but without awareness of how the body responds, rehabilitation becomes a guessing game. I hit a plateau around week six. My motivation dipped. I started skipping sessions, convincing myself that rest was just as important. While rest is essential, unstructured rest without insight can delay healing. It wasn’t until I spoke with my therapist about my frustration that she suggested a simple but powerful solution: start tracking. Not just the exercises, but how I felt during and after them. That conversation marked a turning point. I realized that recovery isn’t only physical — it’s mental and emotional, too. And like any meaningful process, it benefits from observation and intention.
Why Tracking Matters in Rehabilitation Training
Rehabilitation is not a linear process. The body heals in phases, and progress often comes in small increments that are easy to miss without close attention. Tracking transforms invisible changes into visible data, helping individuals stay connected to their recovery. When you monitor symptoms, movement, and effort, you create a feedback loop that informs your actions. This awareness allows for timely adjustments, prevents overuse injuries, and reinforces positive behaviors. Studies in physical therapy consistently show that patients who actively monitor their progress report higher adherence to treatment plans and better functional outcomes.
From a physiological standpoint, the body adapts gradually to movement through a process called neuromuscular re-education. After an injury, neural pathways that control muscle coordination can weaken or become disrupted. Repetitive, mindful movement helps retrain these connections. However, this retraining works best when performed with consistency and precision. Tracking supports this by ensuring exercises are done correctly and at the right intensity. For example, noticing that pain increases after certain movements allows a person to modify their approach before inflammation sets in. Similarly, recording improvements in range of motion reinforces motivation, making abstract goals feel tangible.
Moreover, tracking bridges the gap between clinical visits. Most patients see their physical therapist once or twice a week, leaving several days of self-directed care in between. Without a monitoring system, it’s easy to drift off course. Daily logs act as a personal health journal, offering both the patient and the therapist valuable insights during follow-up appointments. This shared understanding enhances communication and leads to more personalized care. In essence, tracking turns passive recovery into active healing — a shift that empowers individuals to become partners in their own rehabilitation.
What I Actually Monitor — And Why It Works
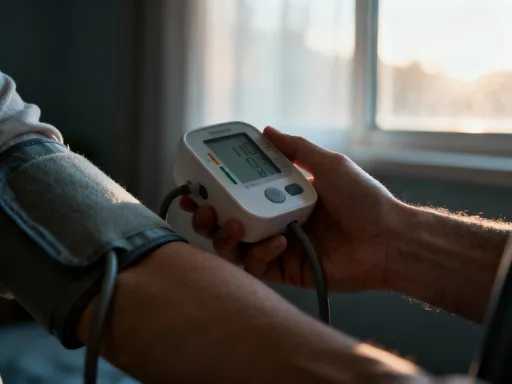
I began by identifying the key indicators that reflected my recovery. These included pain levels, range of motion, energy, mood, and exercise completion. Each morning, I spent five minutes jotting down how my knee felt on a scale from one to ten, noting any stiffness or discomfort. I used a goniometer app on my smartphone to measure the degree of bend in my knee while performing a seated leg lift. Though not medical-grade, the app provided a consistent way to compare results over time. I also observed how easily I could perform basic tasks like standing from a chair or climbing stairs, rating my mobility on a simple scale.
Energy and mood might seem unrelated to physical recovery, but they play a crucial role. Fatigue can signal overexertion, while low mood may reflect frustration or pain accumulation. By logging these factors, I began to see patterns. For instance, days with higher energy often followed better sleep, and those were the days I made the most progress in therapy. Conversely, when I pushed too hard one day, the next day usually brought increased pain and lower motivation. These observations helped me pace myself more effectively. I used a simple notebook at first, then transitioned to a digital journal for easier organization and graphing.
The real power of monitoring came from reviewing the data weekly. Instead of focusing on day-to-day fluctuations, I looked for trends. A slight improvement in knee flexion over two weeks might seem insignificant in isolation, but when plotted on a chart, it became evidence of progress. This long-term perspective reduced anxiety and kept me committed. I stopped chasing dramatic changes and learned to appreciate small wins. Over time, this practice shifted my mindset from impatience to patience, from doubt to confidence. Monitoring didn’t make recovery faster, but it made it more predictable and less overwhelming.
My Simple 5-Step Routine for Daily Check-Ins
To make tracking sustainable, I developed a five-step routine that took less than ten minutes each day. The first step was the morning stretch test. After getting out of bed, I performed a gentle hamstring stretch and noted how far I could reach. I didn’t force it — the goal was to assess, not improve, on the spot. Next, I conducted a mobility score check. I rated my ability to walk across the room, stand up from a low chair, and bend my knee while seated. Each movement received a score from one to five, with five indicating full ease and one meaning significant difficulty.
The third step involved symptom notes. I recorded any pain, swelling, or tightness, along with potential triggers from the previous day. Was it related to activity, posture, or lack of rest? This helped me identify patterns and make informed choices. Step four was a midday movement reminder. I set an alarm on my phone to pause every few hours, stand up, and do three to five minutes of light movement — a short walk, shoulder rolls, or ankle pumps. This prevented stiffness and improved circulation. I also used this time to check my posture, especially when working at a desk.
The final step was evening reflection. Before bed, I reviewed my notes and asked myself: What improved today? What felt harder? Why? I didn’t seek perfect answers, but this brief mental review helped me connect actions with outcomes. Over time, this routine became second nature. It didn’t require special skills or equipment, yet it provided clarity and structure. Most importantly, it gave me a sense of control during a period when I often felt powerless. By anchoring my day to these small, consistent actions, I built a rhythm that supported steady recovery.
How Small Data Adds Up to Big Gains
One of the most encouraging moments in my recovery came two weeks in, when I noticed my knee flexion had increased by ten degrees. On its own, that number might seem minor, but in the context of rehabilitation, it was significant. It meant I could bend my knee further without pain, which translated to greater independence in daily activities. More importantly, it proved that my efforts were working. That small victory boosted my confidence and reminded me that progress doesn’t have to be dramatic to be meaningful.
Another pattern I observed was the link between sleep quality and rehab performance. On nights when I slept well, my pain levels were lower, my energy was higher, and my mobility scores improved. This prompted me to prioritize sleep hygiene — setting a consistent bedtime, reducing screen time before bed, and using a supportive pillow for leg elevation. As my sleep improved, so did my recovery. I also noticed that flare-ups rarely happened without warning. Subtle signs like increased stiffness, mild swelling, or fatigue often preceded a setback by a day or two. By paying attention to these early signals, I could adjust my activity level and prevent a full recurrence of symptoms.
These insights transformed how I approached recovery. Instead of reacting to problems after they arose, I began to anticipate them. I learned to celebrate incremental gains rather than waiting for a grand milestone. This shift in perspective reduced frustration and increased resilience. The data didn’t lie — even on days when I felt stuck, the numbers often showed subtle progress. Over time, the accumulation of these small improvements led to major functional gains. I regained the ability to walk without a limp, climb stairs without holding the railing, and eventually return to light exercise. None of it happened overnight, but each step was documented, validated, and valued.
Tools That Help Without Overcomplicating Things
While a notebook and pen were sufficient at first, I gradually incorporated simple tools to enhance accuracy and convenience. A fitness band became one of my most useful aids. It tracked my heart rate, daily steps, and sleep patterns — all of which provided indirect clues about my recovery. For example, a higher resting heart rate one morning signaled that my body might be under stress, possibly from overexertion the day before. This prompted me to take a lighter approach to my exercises that day. The step count helped me maintain a baseline of activity without overdoing it.
I also used free symptom-tracking apps designed for chronic pain and rehabilitation. These allowed me to log pain levels, mood, and exercise completion with just a few taps. Some apps generated weekly reports, which I shared with my physical therapist during appointments. This made our discussions more productive, as we could review trends together and adjust the treatment plan accordingly. I avoided overly complex systems that required constant input or technical knowledge. The goal was simplicity, not perfection.
A stopwatch, mirror, and smartphone were also essential. I used the stopwatch to time how long I could hold a balance position or perform a set of repetitions. The mirror helped me check my form during exercises, ensuring I wasn’t compensating with other body parts. My smartphone’s camera allowed me to record short videos of my movements, which I reviewed later or shared with my therapist. These low-tech tools were inexpensive but highly effective. They empowered me to stay engaged without feeling overwhelmed by technology. I learned that tools should support recovery, not dominate it. When used wisely, they enhance self-awareness without replacing the body’s own signals.
Staying on Track Without Burning Out
Consistency is key in rehabilitation, but so is balance. There were days when I felt tempted to skip tracking, especially when life got busy or progress felt slow. I learned that discipline must be paired with self-compassion. Missing a day of logging or a therapy session didn’t mean failure — it meant I was human. The important thing was to return to the routine without guilt. I adjusted my expectations based on how I felt, not on an arbitrary timeline. Some days called for rest; others allowed for gentle advancement. Listening to my body became just as important as following the plan.
I also redefined what success looked like. Instead of focusing solely on physical milestones, I celebrated behavioral ones — like completing a week of daily tracking or noticing a pattern in my symptoms. These achievements reinforced positive habits and kept me engaged. I avoided comparing my journey to others, recognizing that recovery is deeply personal. What worked for someone else might not work for me, and that was okay. I stayed focused on my own progress, no matter how small.
Over time, the daily check-ins evolved from a recovery tool into a lifelong habit. Even after I completed formal therapy, I continued to monitor my movement and energy levels. It helped me maintain the gains I had made and prevented future injuries. More than that, it taught me to be more present in my body — to notice, appreciate, and care for it in a way I hadn’t before. The discipline of tracking became a form of self-respect.
Rehab isn’t just about fixing an injury — it’s about rebuilding confidence in your body. By monitoring my progress daily, I stopped guessing and started growing. These small, practical steps didn’t give me instant results, but they gave me control. And that made all the difference. Always remember: this journey is personal, and while self-tracking helps, professional guidance should always lead the way.